Healthcare Learning Management System: Tracking Continuing Medical Education
In the medical field, continuous learning is not optional — it is the foundation of safe, effective, and compliant care. Physicians, nurses, pharmacists, and other professionals must embark on ongoing education to keep up with medical advancements and changing regulatory requirements. Managing this process at scale, however, is complex and time-intensive.
A healthcare learning management system (LMS) can solve this challenge by centralizing education, automating continuing medical education (CME) tracking, and simplifying compliance. Modern healthcare organizations treat LMS as more than technology — it is a strategic investment in workforce readiness and patient safety.
What is a Healthcare Learning Management System (LMS)?
A healthcare learning management system is a type of software designed specifically for hospitals, clinics, and health systems to manage, deliver, and track staff training.
Unlike general-purpose corporate LMS platforms, a healthcare LMS supports healthcare-specific accreditation requirements, compliance tracking, and clinical workflows. It serves as a single platform for clinicians, administrators, and compliance officers to coordinate education.
At its core, a healthcare LMS provides structured course management, role-based learning assignments, certification and CME credit tracking, and analytics. Beyond these essentials, advanced platforms include simulation integration, mobile learning, and interoperability with hospital systems. This combination of features allows organizations to maintain regulatory compliance while also fostering professional development of their staff.
Healthcare LMS users are diverse.
- Physicians use it to complete CME credits.
- Nurses access continuing education modules required for licensure.
- Pharmacists leverage LMSs to meet ACPE requirements.
- Administrators track compliance across departments.
By uniting these roles in one platform, an effective LMS ensures consistent education standards across the organization.
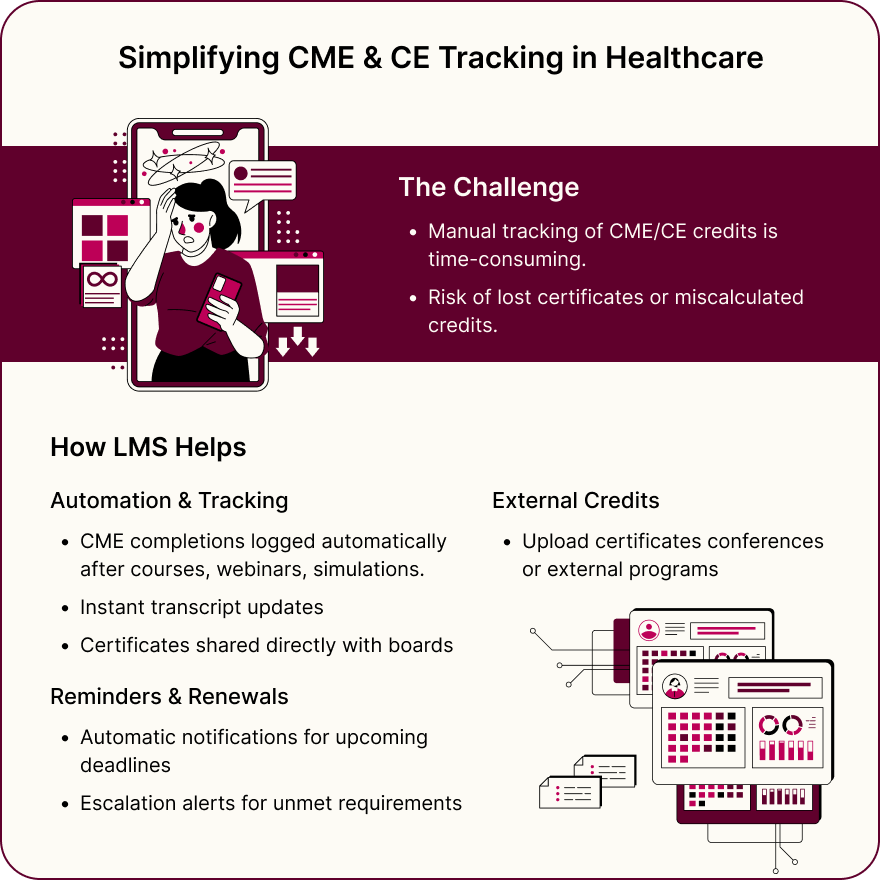
CME and CE Tracking in Healthcare LMS
Tracking continuing education is one of the most important — and most time-consuming — tasks in healthcare training. Clinicians must earn CME and CE credits regularly to renew licenses, maintain certification, and enjoy a good reputation with accrediting bodies. A healthcare learning management system automates this process, making it far easier to manage across large organizations.
Instead of relying on spreadsheets or manual record-keeping, the LMS records CME completions automatically. When a physician finishes an online course, attends a webinar, or participates in a simulation, their credits are logged instantly in the transcript. Transcripts can be shared directly with boards upon certificate issuance, and administrators can verify compliance at a glance. This innovation removes the risk of lost paperwork or miscalculated credits.
Automation extends to reminders and renewals. The LMS notifies clinicians when they are approaching credit deadlines, and managers receive escalation alerts if requirements remain unmet. This proactive approach helps organizations avoid costly penalties or credentialing delays.
Another advantage is the LMS users’ ability to manage external CME activities. Many clinicians attend conferences or earn credits outside their employing organization. A modern healthcare LMS allows users to upload certificates, which are then verified and added to their transcripts. This way, education records are kept complete and accurate, no matter where the learning occurred.
Key benefits of using an LMS for CME and CE tracking include:
- Automated record-keeping eliminates spreadsheets and paper certificates, ensuring accuracy.
- Credit assignment and transcripts. The LMS tracks CME/CE completions and generates proof for licensing boards.
- Renewal reminders. The system sends notifications before deadlines, preventing lapses in certification.
- External activity uploads allow staff to add credits earned at conferences or external programs.
- Department-wide reporting provides managers with real-time dashboards for compliance visibility.
By integrating credit tracking into the broader learning experience, healthcare LMS platforms reduce administrative overhead and improve compliance visibility. Their adoption transforms continuing education from a regulatory burden into an efficient, structured part of workforce development.
Accreditation and Compliance Requirements
Compliance is one of the biggest challenges in healthcare training, as every professional group must follow strict accreditation rules:
- ACCME requirements for physicians.
- ANCC guidelines for nurses.
- ACPE standards for pharmacists.
A healthcare learning management system addresses this hurdle by embedding standards directly into learning workflows.
An LMS aligns courses with these frameworks, documents activities, and generates audit-ready reports. It also supports mandatory training for HIPAA, OSHA, and specialty-specific requirements, automatically assigning courses based on role or location.
Hospitals face additional complexity with credentialing and privileging procedures, requiring proof that all clinicians are qualified. An LMS simplifies this process with department-wide compliance reports, reducing preparation time for inspections.
Critical compliance functions supported by healthcare LMS platforms include:
- Accreditation alignment. An LMS ensures CME and CE activities meet ACCME, ANCC, and ACPE standards.
- Mandatory training assignment. It automatically enrolls staff in courses required by law or relevant policy.
- Audit readiness. LMSs generate detailed logs and compliance reports for inspections.
- Credentialing support. LMS systems link certifications to job roles, ensuring only qualified staff perform procedures.
- Risk reduction. LMS-enabled compliance monitoring prevents fines, delays, and service disruptions caused by missed requirements.
By embedding accreditation and compliance into daily learning workflows, a healthcare LMS makes regulatory adherence systematic and reliable. This way, clinicians are freed from paperwork, being able to focus on patient care.
Integrations and Interoperability in Healthcare LMS
Healthcare organizations rely on interconnected systems to operate smoothly. An LMS that functions in isolation creates silos and inefficiencies. Therefore, modern healthcare learning management systems emphasize interoperability, allowing training to integrate with existing IT infrastructure.
- HRIS. The most common integration is with HRIS platforms. When an employee is hired, promoted, or transferred, the LMS automatically updates their learning assignments based on job role and department. This way, healthcare organizations eliminate duplicate data entry and ensure training requirements always match responsibilities.
- EHR. Another critical integration is with electronic health records (EHRs). Through standards such as HL7 and FHIR, LMS data can connect directly to clinical workflows. For example, an EHR could restrict access to certain procedures unless the LMS confirms that the clinician’s certification is current. This arrangement reduces errors and improves patient safety.
- Training upgrades. Credentialing and scheduling systems also benefit from integration. If a nurse’s certification expires, the LMS can automatically inform scheduling software to prevent them from being assigned to restricted duties. APIs and webhooks extend this capability, allowing training data to flow into reporting dashboards, data warehouses, and compliance tools.
By creating seamless data flows, healthcare LMS platforms not only reduce administrative effort but also support operational safety. Integration ensures that education is not just tracked for compliance, making it meaningfully connected to healthcare delivery quality.
Learning Modalities and Clinician Engagement
Clinicians have limited time for training, so healthcare LMS platforms must provide flexible and relevant formats that fit into medical professionals’ demanding schedules.The most popular options are as follows.
- Simulation-based learning is particularly effective, allowing clinicians to practice in safe environments using VR, AR, or mannequins, with outcomes tracked for CME credits. Microlearning and case-based modules add further value by delivering short lessons and real-world scenarios that can be completed during shifts.
- Blended models, combining online courses with instructor-led workshops or webinars, ensure both convenience and collaboration. Just-in-time training on mobile devices supports immediate decision-making at the point of care.
By combining these modalities, healthcare LMS platforms make learning practical, accessible, and directly applicable to clinical practice.
Must-Have Features of Healthcare LMS
Not all LMS platforms are created equal. Healthcare organizations require features tailored to their specific compliance, accreditation, and clinical needs. The following are must-have capabilities that define a top-rated healthcare learning management system:
- Accreditation compliance. This feature presupposes built-in alignment with ACCME, ANCC, ACPE, and MOC requirements.
- Automated CME and CE tracking. Certificates, transcripts, and credit renewals should be completed without manual effort.
- Audit-ready reporting. Detailed LMS logs support inspections and credentialing.
- System integrations. HRIS, EHR, and credentialing connections are embedded for seamless workflows.
- Advanced training support. LMSs should enable simulation, VR/AR, microlearning, and blended learning.
- Mobile-first design. Access to courses should be smooth across devices, including smartphones and tablets.
- Security and privacy compliance. HIPAA, SOC 2, and ISO 27001 certifications are mandatory for implementation.
- Analytics and dashboards. Predictive tools should be available for identifying compliance risks.
These features transform the LMS from a simple content library into a strategic platform that supports compliance, safety, and professional development across healthcare organizations.
Conclusion
A learning management system for healthcare is a cornerstone of modern medical education. It centralizes training, automates CME and CE tracking, supports accreditation, and integrates with hospital systems. By providing diverse learning modalities, robust analytics, and strong security, it helps organizations meet compliance standards while improving the competence and confidence of their workforce.
For healthcare leaders, the decision is clear: investing in an LMS is not simply about meeting regulatory requirements. It is about building a culture of continuous learning, reducing risk, and ensuring that every clinician is prepared to deliver the highest standard of care.
Frequently Asked Questions






